Introduction
Dear friends and colleagues. In this second ‘Journal Watch’ Newsletter Dr Alex Manara and Prof Guenter Kirste have identified eight recent publications in deceased organ donation of special interest to the donation community.
There are a wide range of articles in this edition of the Newsletter, covering international consensus statements, policy challenges in India and Africa, in situ and ex-situ donor optimisation, COVID-19 impact, and factors which can influence family agreement to donation. We commend the papers to you.
If you would like to help support the quarterly ‘Journal Watch’ Newsletter, the most important thing you can do is share this newsletter with others from the donation community. If you have published a recent donation related article and would like it considered for inclusion in the next newsletter (no promises), please email dale.gardiner@nhsbt.nhs.uk.
Thank you for reading
Anthony Clarkson
(Director Organ and Tissue Donation and Transplantation, UK; Council Member, ISODP)
Dale Gardiner (Associate Medical Director – Deceased Organ Donation, UK)

Dominguez-Gil B, Ascher N,
Capron AM et al.
Expanding controlled donation after the circulatory determination of death: statement from an international collaborative.
https://link.springer.com/article/10.1007/s0013 -vffx 4-020-06341-7.
Despite the proven potential of controlled donation after the circulatory determination of death (cDCDD) to increase donor numbers and subsequent transplants, this form of donation is practiced in a small number of countries worldwide. This statement from an international collaboration of individuals from donation, transplantation, policy making, law and ethics backgrounds seeks to increase the number of countries practicing cDCDD as a means of moving closer to self-sufficiency in organ donation, and to reduce the reliance on living donors by increasing the deceased donor pool. The paper addresses three steps in the cDCDD pathway that are perceived to be the most likely to raise ethical, legal, professional, or religious objections to the practice of cDCDD in different jurisdictions. First it describes the process of reaching a decision to withdraw life sustaining treatments that can be ethically and legally justified. This decision should be before and independent of any consideration of organ donation and in which transplant professionals must not participate. Second, it establishes the permanent cessation of circulation to the brain as the standard to determine death by circulatory criteria. Death may be declared after an elapsed observation period of 5 min without circulation to the brain to confirm that the absence of circulation to the brain is permanent. Finally, it highlights the value of in situ or ex situ perfusion techniques in increasing the success of cDCDD organ transplantation. It also clarifies that in situ normothermic reperfusion of organs must preclude the restoration of brain perfusion to not invalidate the determination of death.
Marklin GF, O'Sullivan C, Dhar R.
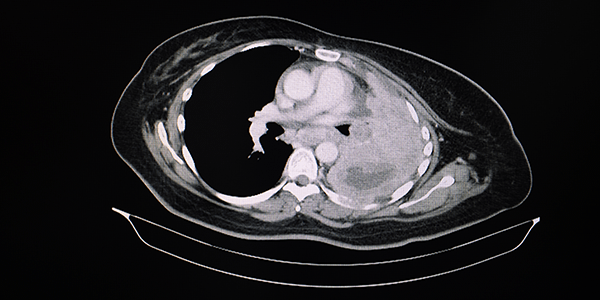
Ventilation in the prone position improves oxygenation and results in more lungs being transplanted from organ donors with hypoxemia and atelectasis.
The value of the prone position as a means of improving oxygenation is now common knowledge following its widespread use during the COVID-19 pandemic. The authors of this paper studied the use of the prone position in consented DBD donors on the PaO2/FiO2 ratio and reduction in atelectasis. Patients in the prone position for 12 hours or longer had significantly more improved PaO2/FiO2 ratio and less atelectasis on CT scan than those left in the supine position. More importantly the utilisation of lungs for transplantation was increased significantly from 24% in the supine group to 45% in the prone group. The study was small (40 patients proned) and difficult to blind, but the results are impressive for a simple, and now well drilled ICU procedure. The impact of this intervention on the family is one issue that needs consideration on a case by case basis.

Shroff S, Gill JS.
Bold policy changes are needed to meet the need for organ transplantation in India.
A thought-provoking viewpoint about the issues that arise in a country with a huge population, an underdeveloped deceased donation programme, and transplantation coming primarily from living donors: 88% of kidney transplants and 77% of liver transplants undertaken in 2019 were from living donors. Transplantation also remains inaccessible to most of the population. The authors explore the root problems and make suggestions on how to develop deceased donation practice and how to increase equity in access to transplantation to all Indians.
van Zanden JE. Leuvenink HGD, Verschuuren EAM et al.
Ex vivo perfusion with methylprednisolone attenuates brain death-induced lung injury in rats.
Methylprednisolone is commonly administered to consented DBD donors to increase the chances of successful lung retrieval and subsequent transplantation. This study in rats went one step further and used methylprednisolone during acellular ex vivo lung perfusion (EVLP) to assess whether it improved the quality of the lungs for transplantation. Lungs treated with methylprednisolone during EVLP showed an increased static and dynamic compliance, and a reduction in lung edema, lactate production and inflammatory mediators in the perfusate. The authors conclude that methylprednisolone during EVLP attenuates brain death induced lung injury. It also demonstrates that ex situ perfusion not only allows assessment of the suitability of organs for transplantation, but also allows interventions that may increase utilisation of organs. A case for a transition from donor optimisation to donated organ optimisation.
Cines DB, Bussel J.
SARS-CoV-2 Vaccine–Induced Immune Thrombotic Thrombocytopenia.
A mass vaccination programme, as the one currently underway for COVID-19 allows the identification of very rare side effects. This editorial describes a new syndrome of vaccine induced thrombosis and thrombocytopaenia (VITT) induced by a recombinant chimpanzee adenoviral vector encoding the spike protein of SARS-CoV-2 (AstraZeneca). The syndrome occurs up to 4 weeks after the first dose of the vaccine and most are women under the age of 50 years. It presents with thrombosis (usually in unusual sites like cerebral venous sinus thrombosis), thrombocytopaenia, raised D-dimer and reduced fibrinogen concentrations. Like heparin induced thrombocytopaenia, it is associated with the presence of anti-platelet factor-4 antibodies even though patients with VITT will not have received heparin. The management of the thrombosis and of the thrombocytopenia should be discussed with haematologists since administration of heparin or platelets may not be appropriate. The relevance to the donation community is that up to 40% of those with the syndrome may die from cerebral thrombosis or intracerebral haemorrhage as a result of the thrombocytopaenia or administration of anticoagulants. These patients may be referred as potential organ donors and it is important to be aware of the possibility of the syndrome as there is the potential of transmitting immune cells that could trigger a similar auto-immune phenomenon in the naive recipient (passenger lymphocyte syndrome). Data on the outcome of transplants from donor with VITTS are very limited but guidance based on expert opinion is available from NHS Blood and Transplant and will be updated as more information becomes available (See Guidance).
Curtis, R.M.K., Manara, A.R.,
Madden, S P et al.
Validation of the factors influencing family consent for organ donation in the UK.
A large database study of 15,465 family approaches in the United Kingdom between April 2014 and March 2019 extracted from the national Potential Donor Audit held by NHS Blood and Transplant to identify factors associated with consent for donation. The consent rate for donation after brain death was significantly higher than for donation after circulatory death, (70% vs. 60%). Knowledge of a patient's donation decision was the factor that increased the consent rate most, but patient ethnicity, religious beliefs, gender and socio-economic status, were also strongly associated with consent (p < 0.001). These factors should be addressed by medium- to long-term strategies to increase community interventions, encouraging family discussions regarding donation decisions and increasing registration on the organ donor register. The most readily modifiable factor was the involvement of a specialist nurse in organ donation at all stages leading up to the approach and the approach itself. When a specialist nurse in organ donation was not present, the consent rates were significantly lower for donation after brain death (OR 0.31, 95%CI 0.23-0.42) and donation after cardiac death (OR 0.26, 95%CI 0.22-0.31) compared to when a collaborative approach was employed. Other modifiable factors that significantly improved consent rates included less than six relatives present during the formal approach; the time from intensive care unit admission to the approach (less for donation after brain death, more for donation after circulatory death); family not witnessing neurological death tests; and the relationship of the primary consenter to the patient. The authors suggest that these modifiable factors should be taken into consideration when planning the best bespoke approach to an individual family to discuss the option of organ donation as an end-of-life care choice for the patient.
Kaul DR, Valesano AL, Petrie JG et al.
Donor to recipient transmission of SARS‐CoV‐2 by lung transplantation despite negative donor upper respiratory tract testing.
A case presentation of the first documented donor to recipient transmission of SARS-COV-2 following lung transplantation. The donor was asymptomatic, and a nasopharyngeal swab was negative on reverse transcriptase polymerase chain reaction (RT-PCR) testing, 48 hours preoperatively. The recipient became symptomatic on the 3rd post-operative day and while nasopharyngeal swab remained RT-PCR negative to SARS-COV-2 the bronchoalveolar lavage sample tested positive. A surgical member present during the transplant procedure also developed COVID-19. Sequence analysis of the isolates confirmed that both the recipient and surgeon’s infection was derived from the donor. Unfortunately, the recipient died 60 days post-transplant. The authors recommend that lower respiratory tract samples should be undertaken in all potential lung donors and that enhanced personal protective equipment for the both the organ recovery team and the transplant team for lung transplantation. No other organs were recovered from the donor. Organ recovery agencies may need to consider whether this advice should be applied to all potential donors, or just to lung donors, particularly during a pandemic.

Lewis A, Kumpfbeck A,
Liebman J et al.
Barriers to the Use of Neurologic Criteria to Declare Death in Africa.
Social
Contact
Address
International Society for Organ
Donation Professionals
c/o The Transplantation Society
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada



