Introduction
Over the past year, the South African journal watch team reviewed a wide range of high-quality, diverse journal articles and benefited from our local academic exchange around them.
The highlight of 2025 was undoubtedly the ISODP conference in Kyoto, Japan. The conference highlighted both global progress and persistent challenges in organ donation systems, reinforcing the importance of multidisciplinary collaboration, ethical clarity, and innovation. We look forward to 2027 in London. Word is there will be a Journal Watch-themed session on that program.
So welcome to Journal Watch - February edition - where we found studies looking to strengthen the efficiency, transparency, and performance of organ donation systems:
-
An article on artificial intelligence-based procurement protocols demonstrated potential to improve specific process intervals, protocol adherence, and data capture, although overall timelines remain unchanged. A study on educational interventions targeting young people shows that knowledge, attitudes, and empathy regarding kidney disease and organ donation can be meaningfully enhanced through creative, experiential learning approaches.
Once again, a paper suggests that legislation alone (opt-out donation frameworks) does not produce sustained improvements in donation rates. Progress likely requires more coordinated public education strategies, supported by healthcare professionals and embedded in everyday clinical and community experiences, to foster informed decision-making and cultural change.
We have a study looking at attitudes toward organ donation in healthcare professionals that are generally positive, but persistent gaps in knowledge regarding legal frameworks, brain death, and donation processes can undermine confidence and affect donation conversations.
Lastly, we have papers that provide physiological and ethical evidence supporting the foundations of current donation practices. Data clarifying the relationship between cessation of cerebral blood flow, brain activity, and systemic circulation support existing donation after circulatory death protocols, while evidence of acceptable outcomes in flexible donation pathways highlights the importance of balancing robust governance with family-centred care.
Collectively, this edition of Journal Watch again demonstrates that advancing organ donation requires a multifaceted approach: technological innovation, public and professional education, ethical clarity, family engagement, and system flexibility.
Dr. Thozama Siyotula
(Pediatric Surgeon)
thozama.siyotula@uct.ac.za
Dr. David Thomson
(Critical Care and Transplant Surgeon)
thomson.david@gmail.com
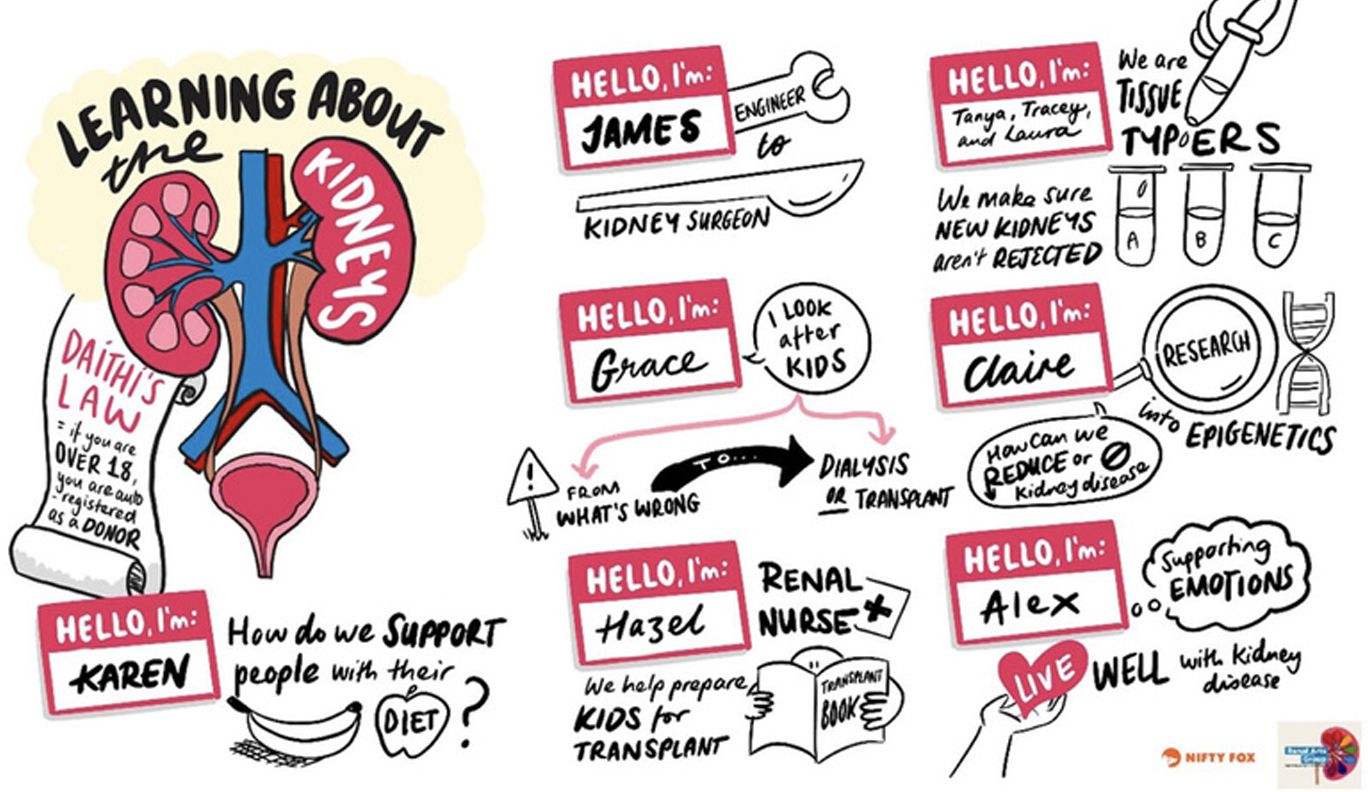
ENGAGING NORTHERN IRELAND SECONDARY SCHOOL STUDENTS ON ORGAN DONATION AND KIDNEY TRANSPLANTATION AWARENESS
McMahona, James et al.
Health Education Journal, November 25, 2025
Corresponding author: James McMahon - j.mcmahon@qub.ac.uk
This article explores the effects of an interactive storyboarding activity on high school students’ knowledge, attitudes and perceptions regarding kidney health and organ donation. Chronic kidney disease (CKD) is now recognized by the World Health Organization as a prioritized non-communicable disease. There is mixed evidence regarding the effectiveness of various renal health awareness interventions internationally.
Using creative, interactive social media interventions is essential to improving health outcomes for youth. This intervention, called “Transplantation Tales”, made use of experiential learning activities supported by renal healthcare professionals and individuals affected by kidney disease.
A pretest-posttest design was used to evaluate changes in teenagers’ knowledge, attitudes, and perceptions. Participants completed the pre-test 1 week prior to attending the event and the post-test within 2 weeks after the workshop.
The use of Storyboarding was seen as a highlight by the learners, and they showed greater empathy after hearing personal stories from individuals affected by kidney disease. The study finding is that young people demonstrated a mind shift regarding their lifestyle behaviours around physical activity and health food choices for reducing the risk of CKD with this intervention. Participants also demonstrated a deeper understanding of CKD, engaged in critical thinking and provided empathic insights during the intervention.
Summary prepared by Barbara Green-Thompson (RN) and Sharon Santon
Family refusal rates for organ donation after brain death and after circulatory death: a single-center 6-year experience
De Min, Federica et al.
Journal of Anesthesia, Analgesia and Critical Care, November 21, 2025
Corresponding author: Martina Baiardo Redaelli - m.baiardoredaelli@uninsubria.it
This study focused on whether family refusal rates differ between donation after brain death (DBD) and controlled circulatory death (cDCD).
The authors conducted a retrospective study using six years of data from five intensive care units at a tertiary hospital in Italy. Patients eligible for organ donation were included, regardless of age.
Most patients lacked prior documented consent, leaving families to decide on their behalf. The results showed that family refusal occurred in 25% of these cases, making it the main reason organ donation did not proceed.
There was no significant difference in consent rates between DBD and cDCD, suggesting that the mode of death did not influence family decisions.
The study highlighted the emotional burden placed on families when consent is not recorded before death. It also showed the importance of encouraging people to register their donation wishes in advance.
Summary prepared by Grant–Lee Hoffman (RN)



Strategic insights into organ donation: perceptions, attitudes, and the impact of disincentive removal in current and future medical professionals
Arizmendi-Villarreal, Marco et al.
Frontiers in Public Health, November 18, 2025
Corresponding author: Francisco Reyna-Sepulveda - francisco.reynas@uanl.edu.mx
In Mexico, when someone has formally agreed to be an organ donor, the final decision still rests with the family. This places healthcare professionals at the heart of difficult, emotional conversations—and makes their knowledge and confidence especially important.
This study explored how prepared current and future healthcare professionals are for this role. Researchers surveyed 686 medical students, residents, and healthcare workers at a university hospital in northern Mexico, asking about their knowledge of organ donation, their attitudes toward donating, and the barriers they believe stand in the way.
The findings show a clear pattern: strong support for organ donation, but an uneven understanding of how the donation system actually works. Most participants were willing to donate organs after death, and many would consider living kidney donation. However,
- Fewer than four in ten correctly identified Mexico’s national transplant authority
- More than half did not realise that families have the final legal say - even when donor wishes are documented and
- Nearly one in ten believed brain death could be reversible, a misconception that can fuel fear and hesitation.
- Concerns about living donation focused on surgical risks, long-term health, and financial costs.
- There was broad support for practical protections for donors, such as covering medical expenses, paid leave, and follow-up care.
Overall, the study demonstrates that positive attitudes are present, but positive attitudes alone are not enough. Better education, clearer policies, and stronger donor support systems are needed to turn willingness into action.
Summary prepared by: Sandra Venter (Tissue Bank Manager)

The relationship between cessation of brain and systemic circulation after withdrawal of life-sustaining measures
Kolisnyk, Matthew et al.
American Journal of Transplantation, October 2025
Corresponding author: Matthew Kolisnyk - amkolisny@uwo.ca
As per Canadian guidelines, death by circulatory criteria (DCC) occurs 5 mins after circulatory arrest. This is grounded in the close relationship among three physiological processes: systemic circulation, brain blood flow, and brain activity.
There is a paucity of evidence on the precise relationship among these three physiological processes and the exact timing of their loss during circulatory arrest. This study aims to address that.
In this single-center, prospective observational trial, they examined the relationship among these three physiological processes in 7 patients who underwent withdrawal of life-sustaining therapy. Measured brain blood flow velocity (BBFv) using transcranial doppler, brain activity using electroencephalography (EEG), and systemic circulation by measuring arterial blood via an indwelling arterial line were reviewed.
The study demonstrated that:
- Brain blood flow stopped before or simultaneously with systemic circulation arrest.
- Brain activity stopped after brain blood flow stopped, but before systemic circulatory arrest.
- Even in cases of sudden cardiac arrest, brain blood flow did not persist beyond circulatory arrest.
This study provided the first direct evidence linking the timing of cerebral blood flow loss, brain activity, and systemic circulation in humans. These findings support the DCD practices in Canada while empirically confirming that both brain blood flow and activity stop before completion of the 5-minute observation period required to determine death using circulatory criteria. It is reassuring that this study links loss of circulation to loss of neurological activity.
Summary prepared by Akhona Mbonisweni

Streamlining organ donation: impact of an artificial intelligence-based protocol post-brain death
Srikanth, ER et al.
BMJ Open Quality, August 26 2025
Corresponding author: Shalini Nair - drshalininair@cmcvellore.ac.in
This study examined whether the introduction of an artificial intelligence (AI) based protocol could improve efficiency and reduce delays in organ procurement following brain death. Conducted at a tertiary transplant centre in Tamil Nadu, India, the authors address a critical challenge in transplantation: prolonged procurement timelines that may compromise organ viability and transplant outcomes.
A retrospective observational study analysed organ donation processes over a five-year period (2018 to 2023). The authors analysed delays across several stages of the procurement pathway, including declaration of brain death, police clearance to transfer to the operating room, duration of surgery, and the interval from completion of surgery to body release. These time points were compared between the pre-AI and post-AI implementation periods.
The AI system was designed to enhance data accuracy, coordination, transparency, and adherence to protocols across the donation pathway. Overall, the study found no statistically significant difference in median total delay times following AI implementation. However, improvements were noted in specific intervals, particularly the time from the first to second apnoea test and from surgery completion to body release. In contrast, a statistically significant increase (p = 0.04) in the time from the first apnoea test to organ recovery was observed after AI adoption. The authors suggest that this may reflect early implementation challenges, including staff learning curves and unfamiliarity with the new system.
Importantly, the study highlights that institutional, legal, and logistical factors, rather than family-related delays, were the dominant contributors to prolonged timelines. The findings highlight the potential of AI to improve data capture, protocol adherence, transparency, and verification in organ procurement processes. At the same time, the study appropriately acknowledges that the impact of AI is context-dependent and that limitations related to infrastructure, training, and workflow integration must be considered when applying such systems across different clinical settings. Ultimately, we have a paper that provides valuable insights into both the promise and the limitations of AI-driven interventions in complex, high-stakes clinical pathways, such as organ donation.
Summary prepared by: Dr Keitumetse Teko-Khoza

Eligible DBD Donors Proceeding via the DCD Pathway: Incidence, Cause, and Outcomes in the United Kingdom
Burgess, Mark et al.
Transplantation Direct, June 12 2025
Corresponding author: Mark Burgess - mark.burgess11@nhs.net
This UK-based retrospective cohort study explores an uncommon but important scenario in organ donation: cases in which patients who met criteria for donation after brain death (DBD) ultimately proceeded through a donation after circulatory death (DCD) pathway. Using national registry data from 2012 to 2022, the authors examined how often this occurred, why it happened, and whether transplant outcomes differed from standard DBD or DCD pathways.
The study found that conversion from an eligible DBD pathway to DCD was rare (approximately 1.5%), highlighting that this is an exceptional rather than routine occurrence. The most common reason for pathway conversion was family preference, particularly a desire for the family to be present at the moment of circulatory arrest. Other contributing factors included clinical instability that prevented completion of the DBD process. These findings underscore the influence of ethical, emotional, and cultural considerations in end-of-life decision-making, even within highly protocolised donation systems.
Importantly, organ utilisation and transplant outcomes were generally comparable between DBD-to-DCD donors and conventional DBD or DCD donors. Kidney utilisation was high, and patient and graft survival outcomes did not differ significantly across groups. While some organ-specific differences were observed such as lower heart utilisation in the DBD-to-DCD group overall transplant success remained acceptable.
The study demonstrates that, although uncommon, DBD donors proceeding via the DCD pathway can yield satisfactory transplant outcomes. It reinforces the importance of flexible, family-centred consent processes supported by robust clinical governance.
Summary prepared by Dr. Thozama Siyotula
Social
Contact
Address
International Society for Organ
Donation Professionals
c/o The Transplantation Society
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada