JUST RELEASED - Transplantation Direct - October 2025 Issue
The October issue of Transplantation Direct is available now for open-access viewing. Several topics are covered in this issue, including quantitative nucleic acid test for BK polyoma virus in kidney transplant recipients; also, biopsy-based transcriptomics variability is compared between kidney transplant centers. In liver transplantation, we feature studies on assessing donor liver quality by testing organ perfusion solution for exosomal small RNA signatures, on how performance status scoring impacts outcomes in obese recipients, on using immune checkpoint inhibitor therapy to downstage hepatocellular carcinoma patients to qualify for transplantation, and on an analysis looking at whether using normothermic machine perfusion can lower costs after DCD transplantation. In addition to these articles, evidence is presented on the use of longitudinal FEV1 measurements as a surrogate for bronchiolitis obliterans evaluation in clinical trials involving lung transplant recipients. On the topic of organ donation, use of DCD donors for simultaneous heart and kidney transplantation is directly compared to using DBD donors. Indeed, we hope that there is something interesting for you in this issue of Transplantation Direct; please visit our open-access website to read all the details.
ISN-TTS Program Application Deadline: October 15
Special ISODP Feature
The International Society for Organ Donation Professionals (ISODP) is dedicated to advancing the field of organ donation worldwide by leading, developing, and supporting professionals as well as fostering best practices. Over the past year, ISODP has undertaken a range of initiatives in pursuit of this mission, notably preparing for the 17th ISODP Congress, which will take place in Kyoto, Japan, from December 3–6, 2025.
This special ISODP edition of the TTS Tribune features perspectives from a former and a current Councilor, who share insight into current developments in living donation and donor care. They also discuss strategies for expanding education and training in organ donation, an endeavor encapsulated by the ISODP Educational Watch initiative, which curates and disseminates targeted learning opportunities to professionals across the globe.


Annual Conference of the Indian Society of Organ Transplantation - October 9-12

We warmly invite all delegates to visit our Executive Director, Marcelle McPhaden at The Transplantation Society (TTS) booth and meet up with the many TTS leaders who will be present. Learn more about TTS, our many initiatives and projects as well as educational and networking opportunities. We look forward to connecting with you at ISOT 2025.
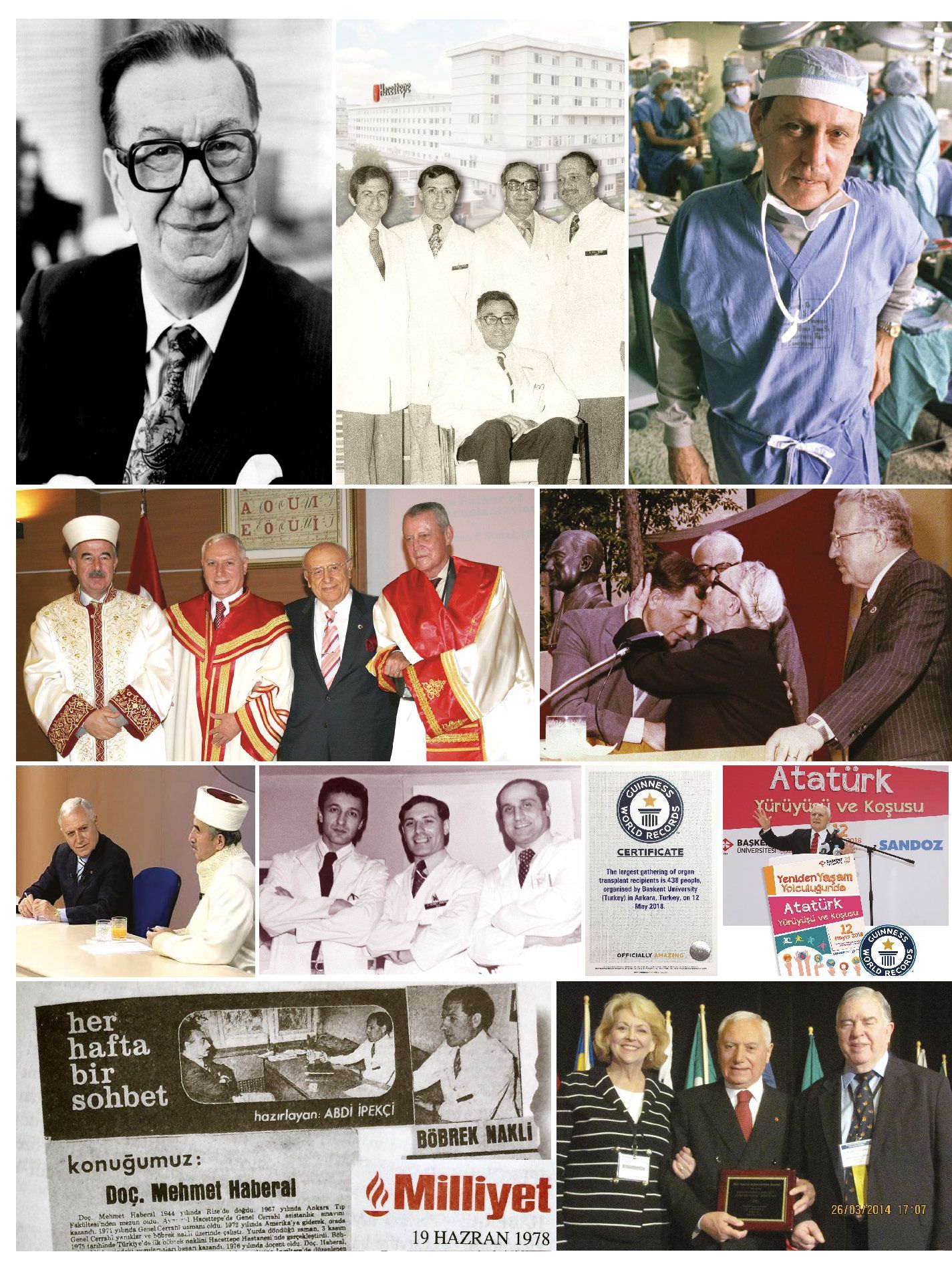
Honoring and Celebrating 50 Years of Organ Transplantation in Türkiye
Ethics and Challenges Involving Uterus Transplantation - Manuscript Published
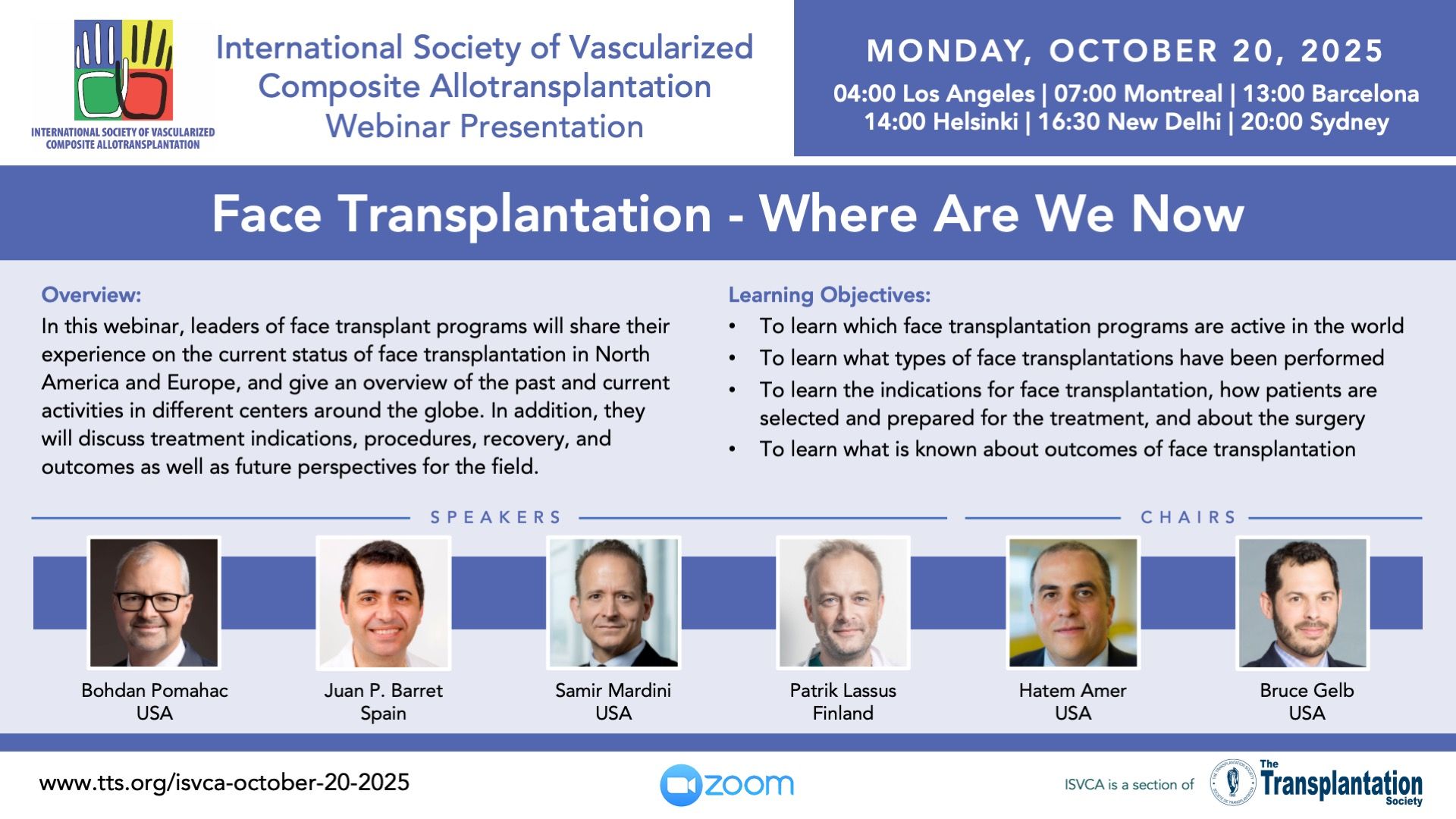
Upcoming Webinar Presentations
2025 Advancing Diversity, Equity & Inclusion in Transplantation Conference - October 25-26
2025 Donate Life Egypt Congress - November 12-15
Asian Transplantation Week 2025 (ATW 2025) - November 20-22
Contact
Address
The Transplantation Society
International Headquarters
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada
Используйте Вавада казино для игры с бонусом — активируйте промокод и начните выигрывать уже сегодня!